How are you study
In Fall 2020, Sinai Health researchers, supported by the Canadian Institutes of Health Research, launched the “How Are You? Survey” to assess the psychological impact of the pandemic on participating staff every quarter for 18 months.
The survey helped to measure the impact of two staff support interventions:
- Peer Resilience Champions who provided mental health support in all areas of the hospital
- Personalized self-awareness feedback provided to a random 50 per cent of survey participants.
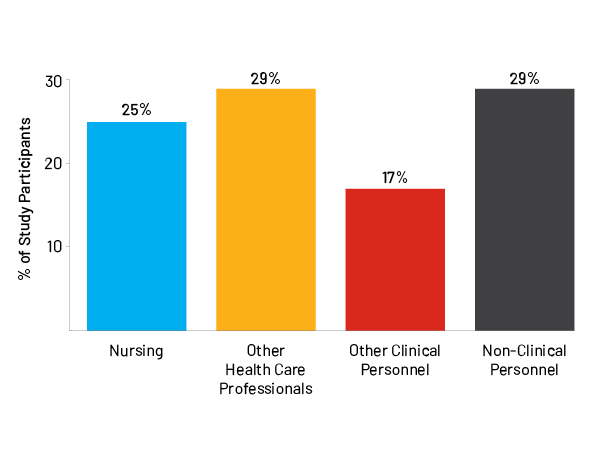
Characteristics of participants
The average age of participants was 38 years, with 33% being 18-30 years, 27% 31-40 years, 23% 41-50 years, and 18% over 50.
79% of participants were female and 57% were married or in common-law relationships.
The racial/ethnic makeup was: European/white (52%), Asian (28%), South Asian (7%), African/Black (6%), Hispanic (3%), and mixed or other ethnicity (6%).
25% were nurses (or students); 29% were other health care professionals (or trainees), 17% had other patient-facing roles, and 29% didn’t have sustained patient contact.
Peer Resilience Champion intervention and resources

Key messages from over 60 groups at Sinai Health who received Peer Champion support.
Desire for:
- Continued transparency around processes
- Continued senior leadership visibility
- Constant attention to maintaining psychological safety
- Training and support in managing interpersonal conflicts at work
Special challenges of the pandemic:
- Tension between what is optimal and what is possible
- Burdens related to staffing
- Recognizing the burden of the pandemic on people of all roles within the hospital
Specific suggestions:
- Pet therapy and massages
Impact of roles and modifiable factors
Burnout was highest in nurses. While other health professionals experienced the next-highest rates of burnout, levels of burnout were concerning in all groups.
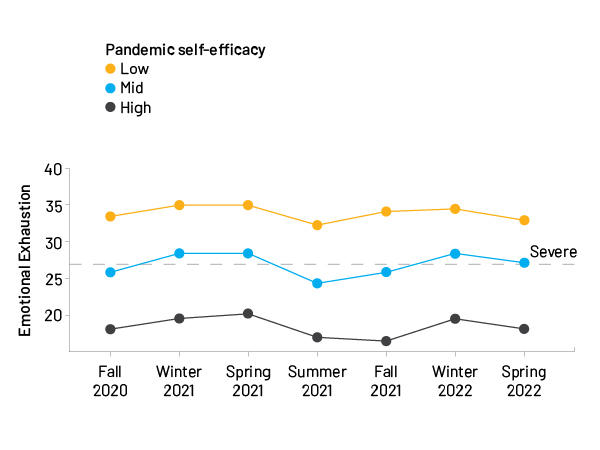
Two factors that can be modified with training were associated with lower burnout.
- Self-efficacy, which is confidence in being able to do a good job. Participants with high self-efficacy had much lower levels of burnout.
- Skills and attitudes that promote resilience, which include maintaining perspective, managing stress, and building networks.
Link to full paper: Psychological impact of the COVID-19 pandemic on hospital workers over time: Relationship to occupational role, living with children and elders, and modifiable factors
Psychological outcomes in relation to COVID-19 case rates
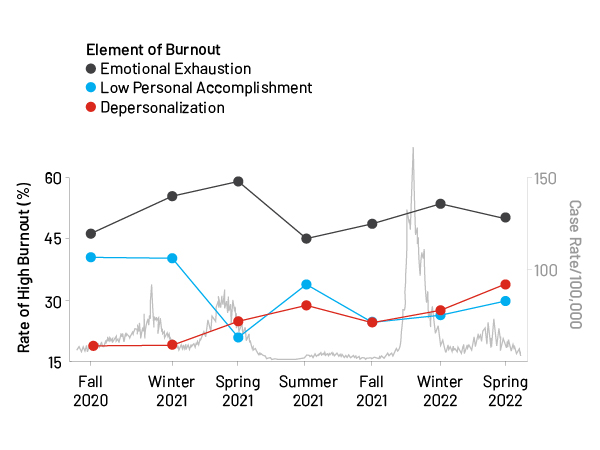
Burnout has three components: emotional exhaustion, a diminished sense of personal accomplishment, and feeling personally disconnected (depersonalization). Of the three components, emotional exhaustion is the most prominent part of burnout for most people.
In the pandemic, levels of emotional exhaustion and personal accomplishment seemed to rise and fall in step with rates of COVID-19 cases. In contrast, rates of depersonalization increased continually, which suggests personal disconnection is a consequence of accumulated workplace stress.
Link to full paper: Trends in burnout and psychological distress in hospital staff over 12 months of the COVID-19 pandemic: a prospective longitudinal survey
Relationships between people and responses to chronic stress
.jpg)
Relationships with other people can reduce the impact of stress when they are going well and can amplify the impact when they are not.
Participants in the “How are You? Survey”, were most likely to report that interpersonal problems resulted from being overly accommodating, self-sacrificing, or over-involved with others (intrusive/needy).
Interpersonal difficulties were related to higher burnout, psychological distress, symptoms of post-traumatic stress and low self-efficacy (lack of confidence).
Link to full paper: Adult attachment insecurity and responses to prolonged severe occupational stress in hospital workers during the COVID-19 pandemic
Morally distressing events
.jpg)
Moral distress arises when circumstances prevent a person from acting in the way they think is morally correct, or when it is not clear what the best moral choice is.
Most survey participants had experienced morally distressing events when we asked in Spring 2021. Nurses and other health professionals had the highest levels of moral distress.
As moral distress goes up, so does burnout.
What survey participants said
Participants in the “How are You? Survey” had an opportunity to write in comments.
Themes emerged that participants emphasized:
- The tension of having to be vigilant during uncertainty.
- The negative emotional impact of COVID-19, balanced against maintaining hope.
- The importance of relationships with colleagues.
- Other stresses related to the pandemic:
- staffing shortages combined with high patient care needs
- polarized views towards public health measures
- feeling devalued
Participants’ comments during the first year of the pandemic





